Please see glossary for defined terms.
Huntington’s Disease, discovered by George Huntington in 1872, is a hereditary genetic brain disorder. Since then, many researchers have dedicated their lives to studying Huntington’s Disease. While we have not found a cure nor treatments to slow the progression, we have discovered how it works, what it is, what it can do, and how it is passed down.
George Huntington, an American physician from Long Island with a degree from Columbia University, published his paper “On Chorea” in 1872, describing Huntington’s Disease so accurately and succinctly that the disease was named after him. He was only 21 when his paper was published. However, he first encountered what would come to be known as Huntington’s Disease when he was 8 years old while accompanying his father and grandfather on medical rounds. Within “On Chorea”, he summarized three key characteristics of a person with Huntington’s Disease: their propensity to suicide and mental disorders, inheritance patterns, and progressive disabilities. This was his sole contribution to medical research. His paper shone a light on this “medical curiosity” from a new field of medicine and shook the medical research world into a frenzy to try to grasp what Huntington’s was and how it worked.
Huntington’s Disease (HD), is inherited from your parents following an autosomal dominant inheritance pattern. It causes nerve cells, mainly in the basal ganglia, brain cortex, and the striatum, to gradually break down and lose function. More than 15,000 Americans currently have HD, but many more are at risk of developing it. There are two kinds of Huntington’s Disease, adult onset, the most common, and early onset, which affects children and teenagers. Fortunately, early onset is very rare, only affecting 5.7% of Huntington’s cases. HD affects an estimated 3 to 7 people out of 100,000, most commonly people of European descent. If a parent has HD, their child has a 50% chance of inheriting the genetic mutation as well. If the child does not inherit it, they will not show symptoms and cannot pass it down. On the condition that the patient has more than 50 CAG repeats, there is a 90% chance they inherited the gene from their father, because CAG repeats tend to be more unstable when passed from the male. There are situations where HD occurs without family history. This event is called Sporadic HD.
Huntington’s is a genetic mutation of the HTT gene. It produces a protein called huntingtin. This protein helps your nerves function. The HTT gene is found on chromosome 4, which also happens to be associated with the cause of many other genetic disorders and some types of cancer. The defect involves a DNA segment known as CAG trinucleotide repeat. It is made up of three DNA building blocks, cytosine, adenine, and guanine, appearing several times in a row. Normally, the CAG segments are repeated 10 to 35 times within a gene, and these people lie in the unaffected range, whether normal or intermediate allele sub-ranges. To a person with Huntington’s, it can be repeated 36 to more than 120 times. They lie in the affected range, either reduced penetrance or full penetrance if they have more than 40 CAG repeats. People in the intermediate allele and the reduced penetrance sub-ranges, with 27-39 CAG repeats, may not develop symptoms but can be carriers. The increase in repeats leads to the production of abnormally long and oddly shaped huntingtin proteins. The elongated protein forms toxic fragments that fuse together and collect in neurons, disrupting the normal function of cells and ultimately killing them. This causes the symptoms of Huntington’s Disease. As the mutated HTT gene is passed down, the amount of CAG trinucleotide repeats increases. A larger number of repeats causes early onset Huntington’s and a sooner appearance of symptoms. This is referred to as anticipation.
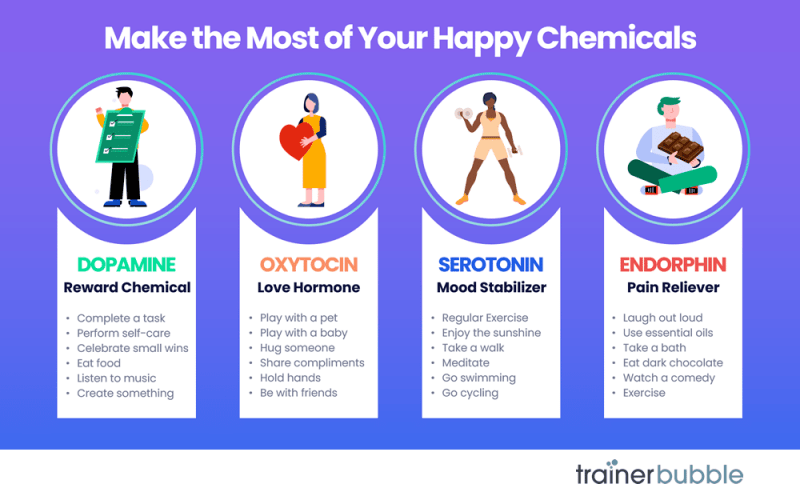
The diverse symptoms of Huntington’s Disease are what leads to many misdiagnoses in the early stages and why it took so long to be recognized as its own disease. George Huntington’s paper “On Chorea” focused mostly on chorea, which involves involuntary jerking or writhing movements, akinesia developing as the disease progresses, unusual or slow eye movements, trouble with walking and balance, dystonia, ataxia, trouble with speech, athetosis, and dysphagia, and weight loss. Mental health conditions include irritability, mood swings, social withdrawal, insomnia, fatigue, loss of energy, suicidal thoughts, OCD, mania, bipolar disorder, psychosis, hallucinations, and paranoia. There are cognitive conditions as well, like, trouble organizing, trouble prioritizing and focusing on tasks, lack of flexibility and perseveration, lack of impulse control that can lead to violent outbursts, lack of awareness in one selves behaviors and ability, slowness in processing thoughts, seizures, trouble with driving, and trouble learning new information and memorization. These symptoms can get more intense when the person is nervous or distracted. Eventually, these symptoms get so bad that it is more closely categorized as dementia.
Many people with HD remain conscious of their environment and can express emotions. As it progresses, the patient will need more help and supervision. Ultimately, they will need help at all hours of the day. HD is not fatal in and of itself. Patients most commonly die from complications like physical injury from falls and accidents, malnutrition due to trouble feeding oneself, infections, typically pneumonia but others as well, choking, heart failure, seizures, and, due to the mental toll, 7-10% of HD patients commit suicide. The average lifespan of a person with Huntington’s is 10 to 30 years after a diagnosis.
This disease, because of its diverse symptoms, takes a skilled eye to diagnose. In most cases, it can be done with a neurological exam and an analysis of the patient’s medical and family history. But in other cases, the patient might require genetic and blood tests and diagnostic imaging like an MRI, CT, PET scan, or EEG. A neurologist and neuropsychiatrist will perform these tests. There are many research studies underway to study Huntington’s and while we do not have a cure, we have a basic understanding of the disease, which means we are one step closer to long term treatments. Johns Hopkins, for example, has 4 ongoing studies: the Sage Studies: PERSPECTIVE Program, which is evaluating the safety and efficiency of the experimental drug SAGE-718 in adults with early Huntington’s Disease, the Generation HD2 tests, which is the second phase of tests on Tominersen in young adults with HD ranging from 25-50 years old. The HDClarity study, an observational study to collect cerebrospinal fluid in order to study biomarkers that influence HD’s pathophysiology and growth, and the Enroll-HD program, a registry for the Global Huntington Disease Cohort, providing vast information for future clinical research. These are just a few of the many programs dedicated to unlocking the mysteries of HD. The most promising fields are those studying biomarkers, like the HDClarity study, and stem cell research.
There are many options for treatments that can help improve the quality of life for a person with HD. They will require more help as the disease progresses and a team of people to help them like a neurologist, psychiatrist, genetic counselor, physical therapist, occupational therapist, and a speech therapist. A counselor could also help the patient and their family members with the emotional toll. Medications can also be prescribed to ease symptoms and keep them functioning as long as possible. To treat chorea they could take deutetrabenazine, amantadine, tetrabenazine, or haloperidol. The latter two of which could also help deter hallucinations and delusions. To manage their emotions, they could be prescribed antidepressants like fluoxetine and sertraline, antipsychotic drugs like risperidone and olanzapine; however, some antipsychotic medications have side effects that could make chorea and akinesia worse, and mood stabilizing medications like lithium. Antidepressant and antianxiety medications are also commonly prescribed because there are high rates of depression and suicide amongst patients with HD. It is also recommended to maintain physical fitness because it is shown that patients who exercise regularly delay the symptoms of HD more than those who do not. Huntington’s, however, can be prevented by genetic counseling, prenatal testing, and in vitro fertilization, where an egg and sperm are fertilized in a lab and checked to see if it has Huntington’s disease. If it does not, it is then implanted back into the uterus. It is important to speak to a genetic counselor before having a child if you or your partner has HD or is at risk to develop symptoms.
An HD diagnosis is certainly not a death sentence. A person with Huntington’s can live a long, happy life. We now know so much about this disease that even George Huntington would not be able to believe. There are many options for every particular patient and every particular case. And as science and technology advances, so will we in our path to finding a cure for Huntington’s Disease.
Glossary
1. A CAG trinucleotide repeat is an unstable expansion of the DNA sequence “cytosine-adenine-guanine” (CAG) that codes for the amino acid glutamine, resulting in a long “polyglutamine” tract within a protein
2. a situation where individuals who inherit a disease-causing genetic mutation do not develop the associated disease or condition
3. Akinesia: become rigid (stiff) and move very little or not at all
4. Dystonia: unusual fixed (unchanging) postures
5. Ataxia: loss of coordination
6. Athetosis: slow, involuntary, and writhing movements
7. Dysphagia: difficulty swallowing
8. Psychosis: losing some contact with reality
9. Tominersen: a treatment for Huntington’s Disease that is under research and trials
References
U.S. Department of Health and Human Services. (2024, December 12). Huntington’s disease. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/huntingtons-disease
Mayo Foundation for Medical Education and Research. (2024, April 25). Huntington’s disease. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/huntingtons-disease/symptoms-causes/syc-20356117
Huntington’s disease: What is it? Cleveland Clinic. (2024, May 1). https://my.clevelandclinic.org/health/diseases/14369-huntingtons-disease
Huntington’s disease. Johns Hopkins Medicine. (2024, June 6). https://www.hopkinsmedicine.org/health/conditions-and-diseases/huntingtons-disease
U.S. National Library of Medicine. (2020, July 1). Huntington’s disease: Medlineplus genetics. MedlinePlus. https://medlineplus.gov/genetics/condition/huntingtons-disease/
Huntington’s disease. ucsfhealth.org. (n.d.). https://www.ucsfhealth.org/conditions/huntingtons-disease
Huntington’s disease – symptoms, causes, treatment: Nord. National Organization for Rare Disorders. (2023, November 20). https://rarediseases.org/rare-diseases/huntingtons-disease/
What is Huntington’s disease? Huntington’s Disease Association – Home. (n.d.). https://www.hda.org.uk/information-and-support/huntingtons-disease/what-is-huntingtons-disease/
Huntington’s Disease Society of America. Huntington’s Disease Society of America – Family Is Everything. (n.d.). https://hdsa.org/
Durbach, N., & Hayden, M. R. (1993, May). George Huntington: The man behind the eponym. Journal of medical genetics. https://pmc.ncbi.nlm.nih.gov/articles/PMC1016378/#:~:text=Abstract,was%20later%20named%20after%20him
Squitieri, F. (2013). Numero verde huntington. LIRH. https://lirh.it/en/history-huntingtons-disease#:~:text=George%20Huntington%20
History of Huntington’s Disease – Huntington’s Disease Society of America. Huntington’s Disease Society of America – Family Is Everything. (2019, March 20). https://hdsa.org/what-is-hd/history-and-genetics-of-huntingtons-disease/history-of-huntingtons-disease/